Antibiotic resistance could result in common infections, such as tonsillitis and otits, becoming difficult to treat in the future and in worst case, even be fatal. Common surgeries and cancer treatments also depend on effective antibiotics.
If the current development continues, by 2050, 10 million lives are at risk every year due to antibiotic resistance (AMR), according to the World Health Organization (WHO). This can be compared to about 8 million people dying of cancer and approximately 1 million people in traffic accidents every year.1
What are antibiotics?
Antibiotics are drugs used to treat infections caused by bacteria. There are different types of antibiotics, antibiotics that affect many different bacteria are considered a broad-spectrum antibiotic while antibiotics that affect only a few bacteria is a narrow-spectrum. Excessive use of antibiotics has led to disease-causing bacteria have developed resistance to the drug.
What is antibiotic resistance?
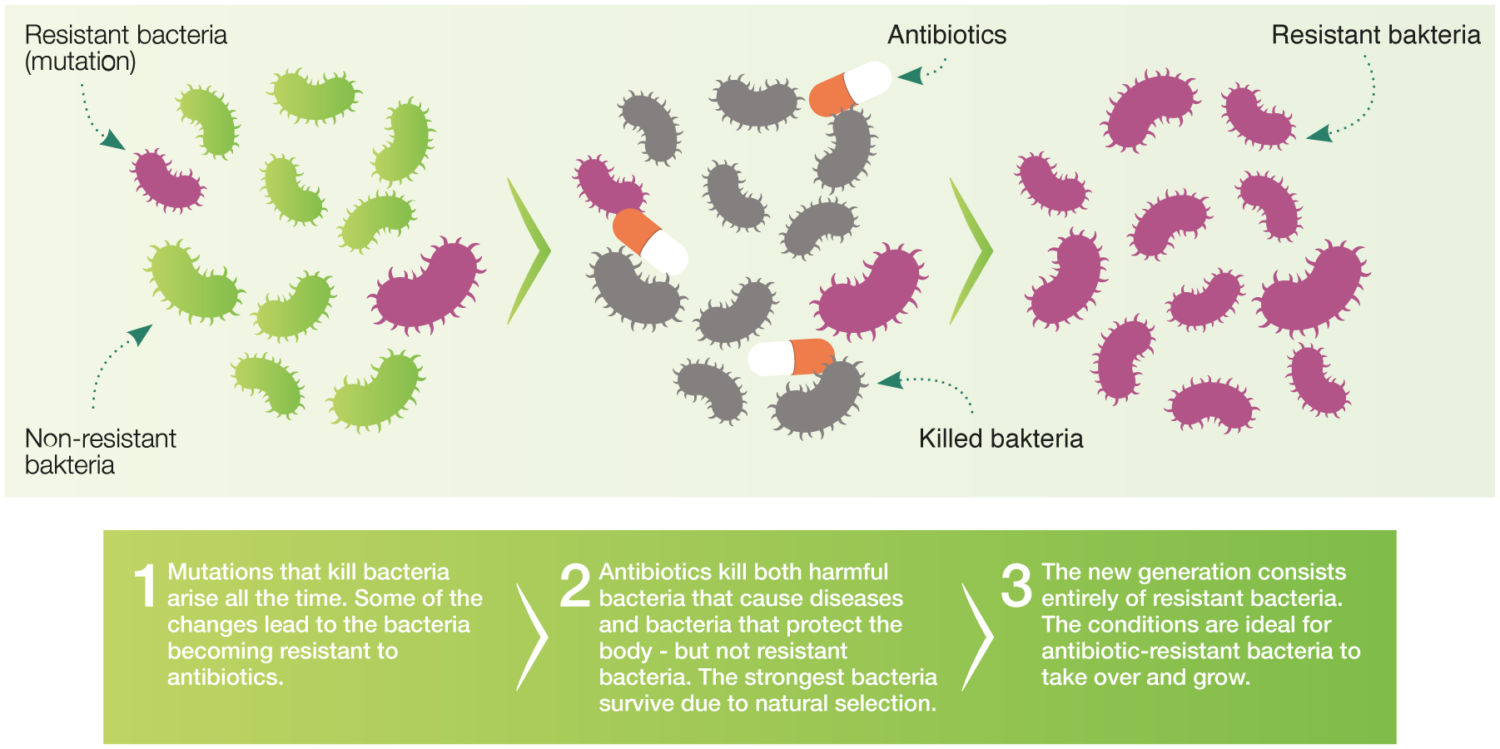
Resistance is the bacteria’s natural way of adapting to its environment in order to survive. When disease-causing bacteria become resistant to antibiotics, the risk increases that an infection takes longer to treat or that the treatment does not work at all. In worst case, the patient dies from the infection. It is important to remember that resistance is a property of the bacteria. A patient being treated with antibiotics cannot become resistant.
How AMR develop
Multi-resistant bacteria or superbugs
When a bacterium becomes resistant to several different types of antibiotics, it is called multi-resistant (in media also often called “superbugs”). Two common terms that are often mentioned in connection with antibiotic resistance and multi-resistant bacteria are MRSA and ESBL.
MRSA
MRSA stands for multi-resistant staphylococci aureus and is yellow staphylococci bacteria that is resistant to certain antibiotics. MRSA does not cause more or more serious infections than common yellow staphylococci, but there are fewer antibiotics to treat the infection with. The staphylococci are most often found in the nose, throat or other mucous membranes. They can also be found on the skin, for example in the groin and armpits.
You can be a carrier of bacteria such as yellow staphylococci on the body without having any problems, being an MRSA carrier gives no symptoms. MRSA is still quite uncommon in Sweden but is more common abroad.
ESBL
Unlike MRSA, ESBL is not a microbe, but a resistance mechanism found in some bacteria. ESBL is an abbreviation for Extended Spectrum Beta-Lactamase which is a group of enzymes that intestinal bacteria can form. The enzymes break down several different types of important antibiotics in the antibiotic group beta-lactams, which means that the antibiotic loses its effect.
Several different intestinal bacteria can form these enzymes, the most common being Escherichia coli (E. coli) and Klebsiella pneumoniae, but ESBL has also been detected in other intestinal bacteria such as Enterobacter, Proteus, Pseudomonas and Salmonella.
The fact that a bacterium has ESBL does not mean that the infected person will becomes sicker than from other bacteria, but the infection might be more difficult to treat. Examples of common infections where ESBL bacteria complicate the process are urinary tract infections and infections that occur after surgery and sometimes blood poisoning.
Bacterial strains that carry ESBL are more common abroad than in Sweden.
Less infections lead to reduced antibiotic use
Less infections will result in a reduction in the use of antibiotics and better health for patients. Every infection prevented, is an antibiotic treatment avoided.
According to the WHO, it is now more important than ever to prevent infections. By preventing infections, we can save millions of lives every year, while reducing the spread of antibiotic-resistant bacteria.
References:
1. European Commission. 2017. A European one health action plan against antimicrobial resistance (AMR).